COLT Project

COLT was created 10 years ago based on an observation: Lung transplantation is the only treatment for patients with chronic end-stage respiratory disease. However, long-term survival remains poor, with 53% survival at 5 years. The main cause of late mortality is Chronic Lung Allograft Dysfunction (CLAD) – CLAD is observed in almost 50% of patients at 5 years post-transplant.
Setting up of COLT
COLT was initiated as a result of the French transplant centers’ determination to join forces to prevent CLAD.
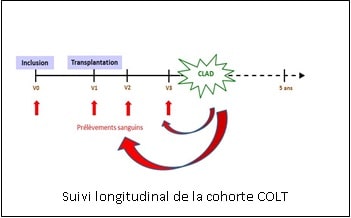
COLT’s main objective is the discovery of early factors which can predict CLAD. The method is the constitution of a cohort whose patients are seen prior to transplantation and then regularly over a period of 10 years. Blood samples are collected at each visit up to 5 years of patient follow-up (figure opposite). The initial objective was to recruit 500 lung transplant patients. Fundings from Vaincre la Mucoviscidose and the Association Gregory Lemarchal in 2008 allowed the project to start. These fundings had a leverage effect to raise additional funds and obtain funding from an Hospital Clinical Research Program (PHRC).
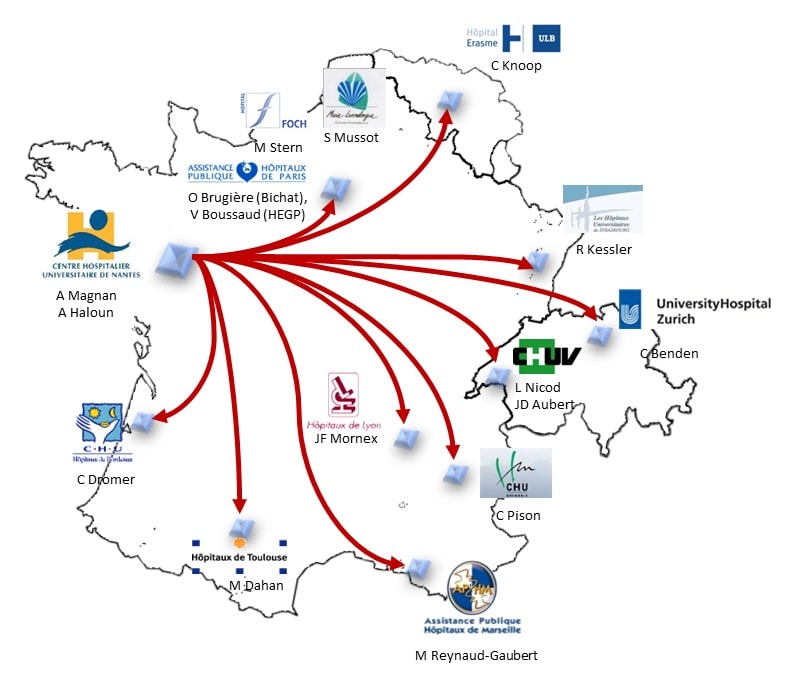
This project, coordinated by the Nantes University Hospital, brought together the 11 French adult lung transplant centers. The first inclusion in COLT took place on September 2, 2009. The inclusion targets of 500 transplanted patients were reached in March 2011, but the success of this collective work has motivated the centers to continue the project. During 2012, the integration of the Erasmus Hospital (Brussels, Belgium) as the 12th center allowed the cohort to open up internationally. In 2012, the COLT cohort also joined forces with the Swiss Cohort STCS and French and European start-ups around a common project: SysCLAD (Systems prediction of chronic lung allograft dysfunction). The aim was to use some of the data and samples collected since 2009 in COLT, but also by our Swiss colleagues, to provide CLAD modeling through the integration of clinical and biological data.
Results :
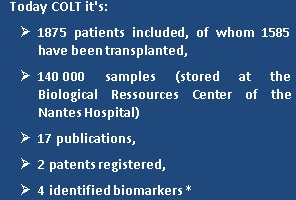 Several major progresses have been made with the identification by Nantes research teams of 4 CLAD predictive blood biomarkers. A transcriptomic analysis identified 3 genes (POU2AF1, BLK and TCL1A) under-expressed 6 months before the diagnosis of CLAD. The study of white blood cells and in particular blood lymphocytes revealed a higher frequency of regulatory T lymphocytes in patients who would subsequently develop CLAD and, on the contrary, in stable patients (i.e. without CLAD at 3 years post-transplant) a higher proportion of regulatory B lymphocytes. Finally, MMP-9, a protein involved in fibrosis and bronchial remodeling, was found at higher levels in CLAD patients almost 12 months prior to clinical diagnosis. We can also report as a highlight the identification of the deleterious role of air pollution on the respiratory function of lung transplant patients (Grenoble team).
Several major progresses have been made with the identification by Nantes research teams of 4 CLAD predictive blood biomarkers. A transcriptomic analysis identified 3 genes (POU2AF1, BLK and TCL1A) under-expressed 6 months before the diagnosis of CLAD. The study of white blood cells and in particular blood lymphocytes revealed a higher frequency of regulatory T lymphocytes in patients who would subsequently develop CLAD and, on the contrary, in stable patients (i.e. without CLAD at 3 years post-transplant) a higher proportion of regulatory B lymphocytes. Finally, MMP-9, a protein involved in fibrosis and bronchial remodeling, was found at higher levels in CLAD patients almost 12 months prior to clinical diagnosis. We can also report as a highlight the identification of the deleterious role of air pollution on the respiratory function of lung transplant patients (Grenoble team).
The future of COLT is in the short term the PRELUD project, which aims to validate the biomarkers identified (above), to combine them to obtain a predictive CLAD score and to validate this score in a new prospective cohort attached to the COLT cohort.
* Tissot A et al. COLT : 10 ans de recherche en transplantation pulmonaire, résultats et perspectives. Rev Mal Respir. 2018 Sep;35(7):699-705.
