News & Highlights

Background :
Interleukin-7 (IL-7) is the most important cytokine for T-cell homeostasis. IL-7 signals through the IL-7 receptor (IL-7R) which is composed of an alpha chain (IL-7Rα), also called CD127 and a common gamma chain T lymphocytes, especially T helper type 2, play a crucial role in the pathobiology of allergic asthma
Objective :
To study the effects of an anti-CD127 monoclonal antibody (mAb) in a murine model of allergic airway inflammation induced by house dust mite (HDM).
Methods :
Allergic airway inflammation was induced in mice using a protocol comprising 4 weekly percutaneous sensitizations followed by 2 weekly intranasal challenges with total HDM extracts and treated by intraperitoneal injections of an anti-CD127 mAb. Because CD127 is shared by both IL-7R and the receptor for thymic stromal lymphopoietin (TSLP), a group of mice was also treated with an anti-IL-7 mAb to block only the IL-7 signaling pathway.
Results :
Anti-CD127 mAb-treated mice showed significantly lower airway resistance in response to methacholine and improvement in lung histology compared with isotype mAb-treated animals.
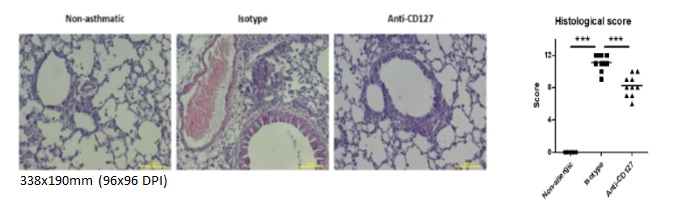
Figure 1 : Treatment with anti-CD127 antibody improves lung histology in a mouse model of house dust mite induced allergic asthma. (A) Representative microphotography showing a decrease in bronchial epithelial cell hyperplasia and inflammatory infiltrate in the lungs of mice treated with anti-CD127 antibody compared to those treated with the isotypic control antibody (hematoxylin and eosin staining, original x200 magnification). B) The improvement in histology is confirmed by a semi-quantitative histological score. ***p<0.001, each point represents a mouse.
Anti-CD127 mAb treatment significantly decreased the mRNA expression of Th2 cytokines (IL-4, IL-5, and IL-13) and chemokines (CCL5/RANTES) in lung tissue, decreased the secretion of Th2 cytokines (IL-4, IL-5, and IL-13) and chemokines (CXCL1 and CCL11/eotaxin) in bronchoalveolar lavage fluid (BALF), decreased serum HDM-specific IgE, and reduced the number of total leucocytes and leucocyte subpopulations such as eosinophils, macrophages, lymphocytes, T lymphocytes, and ILC2 in BALF and lung tissue. Mice treated with anti-IL-7 mAb also showed less allergic airway inflammation as evidenced by significantly lower airway resistance and fewer leucocytes in BALF and lung tissue compared to mice treated with the corresponding isotype control mAb.
Conclusion :
Targeting the IL-7Rα by an anti-CD127 mAb improves allergic airway inflammation in mice and presents as a potential therapeutic approach for allergic asthma.
