Respiratory diseases

Respiratory pathologies covered at the Nantes University Hospital
All adult respiratory diseases are treated in the respiratory medicine Department of the Nantes University Hospital, without exception. The main diseases investigated and treated in the department are: pulmonary aspergillosis, asthma, chronic obstructive pulmonary disease (COPD), lung and pleural cancers, bronchiectasis, pulmonary embolism, emphysema, pulmonary arterial hypertension, obstructive or restrictive respiratory insufficiency, legionellosis, diseases related to asbestos or other exposures, cystic fibrosis, pulmonary mycobacteriosis and tuberculosis, diaphragmatic paralysis, pleurisy, pneumonia, diffuse interstitial lung diseases, pneumothorax, sarcoidosis, sleep apnea syndrome, obesity-hypoventilation syndrome and chronic cough.
The Department also contributes to the respiratory management of rarer diseases, but the exhaustive list would be too long to establish. Examples include allergic bronchopulmonary aspergillosis, ciliary dyskinesias, Langerhansian histiocytosis, pulmonary lymphangioleiomyomatosis, respiratory manifestations of connective tissue disease, myopathies, alveolar proteinosis, Birt Hogg Dubé syndrome and vasculitis.
The most common signs leading to the discovery of these diseases are: shortness of breath (dyspnea), cough, sputum, spitting blood (hemoptysis), chest pain, weight loss, fever. Depending on the symptoms and the data of the consultation, several types of complementary exams are generally proposed: chest X-ray, chest CT scan, MRI, bronchial fibroscopy, respiratory functional exploration, 6-minute walk test, sleep recording (most often on an outpatient basis), respiratory effort test, venous or arterial blood tests (blood gas), sputum analysis, pleural puncture, pleural biopsy, echocardiography, electrocardiogram.
Consultations are provided Monday to Friday from 8:30 am to 6:30 pm.
Asthma
Asthma is the world’s leading chronic respiratory disease, with approximately 4.5 million people affected in France. This disease results in chronic inflammation of the lower airways, bronchoconstriction and bronchial hypersecretion, associated with bronchial remodeling. Inhaled corticosteroids are the cornerstone of asthma treatment, combined with short-acting and sometimes long-acting bronchodilators. Severe asthma affects approximately 5 to 10% of asthmatics and is responsible for a disabling disease with a strong impact on quality of life and multiple unexpected hospitalizations. A better understanding of asthma pathophysiology has highlighted different phenotypes (Cf. figure below).
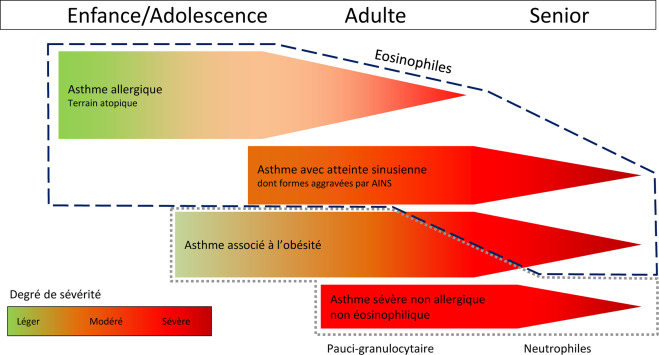
Hassoun D et al. Rev Med Interne, 2019
Thus, new therapies have emerged over the last ten years, such as antibodies directed against IgE for allergic phenotypes, or against interleukin 5 (IL-5), IL-4 or IL-13 for eosinophilic TH2 phenotypes. These biotherapies (monoclonal antibodies) are now an integral part of the therapeutic strategy.
However, for patients with a non-TH2 non-eosinophilic phenotype, no effective biotherapy has been found to date, exposing patients to long-term oral corticosteroid therapy with many side effects.
Other therapeutic approaches such as bronchial thermoplasty have demonstrated a beneficial effect in some patients with a significant part of bronchoconstriction in their disease. Although many breakthroughs have been made in recent years, fundamental and clinical research remains essential in this pathology.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (also known as COPD) is a disease of the lung. By far the most common cause is smoking. But there are also cases related to exposure to toxic products, smoke, gas, vapors or dust (usually of occupational origin). This disease causes a narrowing of the airways called bronchial obstruction and also a destruction of the lung parenchyma leading to the formation of holes in the lung called emphysema. COPD is a frequent disease. It is estimated that it affects about 3 to 3.5 million people in France, a very large proportion of whom are unaware that they have it.
The disease evolves progressively, sometimes over several years. At the beginning, it is just a simple shortness of breath during effort, which can then worsen over the years. Eventually, the lack of air can be felt even at rest. Coughing and spitting are often present at baseline and can be increased notably when respiratory infection occurs (these episodes are called exacerbations causing a major. Diagnosis is based mainly on measurements of breathing, known as functional respiratory explorations. This test measures bronchial obstruction by a measured value called FEV1 (maximum exhaled volume in 1 second).
The treatment of this disease is mainly based on stopping smoking. This cessation can be facilitated with the help of specialized doctors called tabacologists.

Influenza vaccination is essential in the case of COPD. It is also recommended to be vaccinated against pneumococcus.
The main medications for COPD symptoms are called bronchodilators. Their purpose is to open up the bronchi to allow air to pass through the airways.
In the more advanced stage of the disease, if symptoms persist and if there are frequent periods of worsening (exacerbations) despite bronchodilator treatment, inhaled corticosteroids are added.
Respiratory rehabilitation may also be offered to fight against breathlessness and improve quality of life. It combines exercise training, education on healthy living, educational programs for self-management of an exacerbation, monitoring of prescriptions, dietary and psychosocial care.
Oxygen treatment is used only at the stage of chronic respiratory insufficiency, i.e. when the oxygen in the blood, and therefore in the tissues, is not sufficient because of the severity of the respiratory disease.
Cystic Fibrosis
Cystic fibrosis is the most common lethal genetic disease in Caucasian populations. It is related to a CFTR protein defect that is responsible for damage mainly to the upper and lower airways, the digestive, pancreatic and hepatic systems. Cystic fibrosis-related lung disease is responsible in the majority of cases for early mortality and morbidity with coughing and permanent bronchopulmonary congestion, frequent occurrence of respiratory exacerbations requiring antibiotic cures.
Several thousands of mutations have been identified to date. They are grouped according to the types of abnormalities in CFTR protein function that they cause (no synthesis, altered transport to the membrane, etc.).
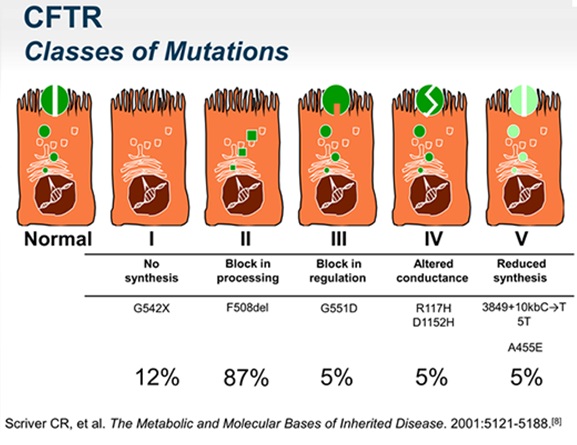
This disease naturally evolves towards lung destruction and chronic respiratory insufficiency, leading to lung transplantation in most cases. The “classic” treatment of cystic fibrosis can be grouped into 3 areas: bronchial drainage by respiratory physiotherapy and the use of aerosols that fluidize bronchial secretions, anti-infectious treatments that can be administered per os, intravenously or inhaled, and pancreatic or nutritional replacement treatments. The median life expectancy of patients has been rising steadily in France since the 1980s thanks to early detection, the use of antibiotics effective against often resistant respiratory germs and the comprehensive care provided by the emergence of cystic fibrosis resources and skills from centers throughout the country. A new, revolutionary step is being taken with the arrival of modulating treatments with Ivacaftor since 2012, Ivacaftor/Lumacaftor since 2016 and since the end of 2019 with temporary authorization for named use Ivacaftor/Tezacaftor/Elexacaftor. These treatments allow partial restoration of CFTR function and have a systemic action with improvement of respiratory function, reduction in the number of exacerbations and weight gain. Albeit they apply to patients with specific mutations, more than 80% of them could benefit from these treatments in the near future. The potential long-term improvement in the prognosis and notably the life expectancy of patients eligible for these drugs is considerable.
Lung Transplantation
Lung transplantation is the only possible treatment for patients with severe chronic respiratory disease. The main diseases leading to discussion of a lung transplant project are chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis and cystic fibrosis. France is a very active country in this field with nearly 400 procedures per year out of a little over 4500 performed worldwide. This therapy is offered to increasing number of patients every year for two reasons. Firstly, the number of grafts available and proposed to the transplant teams has considerably increased thanks to the use of so-called “extended criteria” donor lungs and the implementation of ex vivo reconditioning procedures for lungs initially incompatible with transplantation.

Lung Reconditioning by Ex Vivo Lung Perfusion
Secondly, the last decades have witnessed a constant increase in the life expectancy of transplant patients due to improved surgical and anesthesia-reanimation techniques and better of immunosuppressants and infections management. As a result, lung transplantation is now considered a reliable strategy, with a raising awareness by the general public and more patients have now the opportunity to meet with a transplant team to discuss a transplant project.
However, despite these spectacular improvements, the long-term survival of lung transplant patients remains limited by the frequent occurrence of chronic lung allograft dysfunction (CLAD). CLAD mechanisms are still poorly determined and there is currently no effective treatment against CLAD other than retransplantation. This is probably the main current challenge in pushing the limits in terms of patient’s survival and quality of life. The other remaining challenge to achieve is to build personalized medicine in transplantation, which will provide physicians and patients with potentially revolutionary tools to deal with this highly complex situation integrating immunological interactions, underlying pathology, environment and multiple treatments.
Thoracic oncology
Lung cancer is the leading cause of cancer mortality in France. In terms of incidence, lung cancer is the third most common cancer, with approximately 45,000 new cases diagnosed each year. The majority of lung cancers are linked to tobacco intoxication. Professional risk factors are found in 15% of lung cancers: asbestos, chromium, nickel, radon and other heavy metals.
Among the environmental factors, passive smoking is reported but also exposure to radon, X-rays, diesel engine emissions, air pollution, etc…
There is currently an increasing number of lung cancers, particularly in women, that are not related to tobacco or professional risk factors. They account for 20% to 30% of lung cancers in women and less than 10% in men.
Lung cancers are divided into two main groups: Non-small cell lung cancers and small cell lung cancers.
- Non-small cell lung cancers (NSCLC) : These are the most common lung cancers, accounting for about 85% of cases. Several histological subtypes of non-small cell lung cancers are described: adenocarcinomas (50% of all cancers), squamous cell lung cancers (25% of all cancers).
- Small cell lung cancers : These are neuro-endocrine tumors that account for approximately 15% of lung cancers and are almost exclusively related to very strong tobacco intoxication.
- Other tumors are much rarer such as large cell neuroendocrine tumors or carcinoid tumors.
The Thoracic Oncology Unit of Nantes University Hospital with its team of clinician-researchers, clinical research assistants, and clinical research nurses, participates in numerous national and international clinical trials to treat lung cancer.
Hospital-Acquired Pneumonias
Hospital-acquired pneumonia (HAP) is a major infectious disease worldwide and the most frequent cause of nosocomial infections, with 500,000 episodes treated each year in Europe.
Currently, strategies for the prevention and treatment of HAPs are primarily aimed at reducing the bacterial load, in particular through the use of antimicrobial treatments. PAHs are the main causes of antibiotic consumption in European hospitals and are increasingly induced by drug-resistant pathogens, leading to higher medical costs, longer hospital stays and increased mortality. Developing new alternative treatments and more effective strategies is therefore necessary to fight against the dangerous resistance to antibiotics.
